Flu still prevalent, COVID-19 rates dropping in Mass.
Flu season is at its peak. State health officials say it has been one of the worst seasons. Rates for other respiratory diseases are low, however.
It’s been one of the worst flu seasons in the U.S. in recent memory, but in Massachusetts only last year was worse.
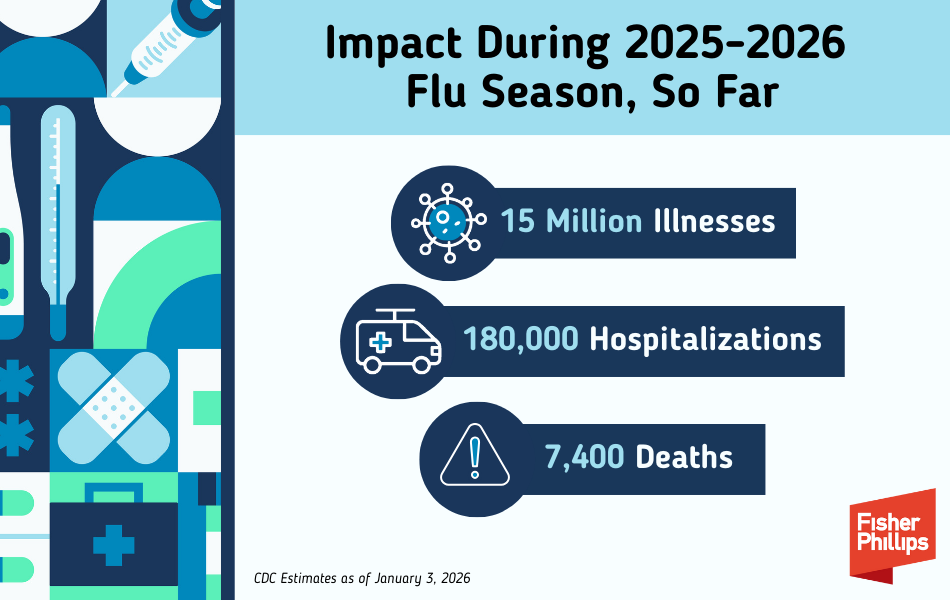
The American Association of Medical Colleges found that “at least 19 million Americans have come down with the flu — and 10,000, including 44 children, have died from the illness — during the 2025-26 flu season so far, making it one of the most brutal in recent memory.”
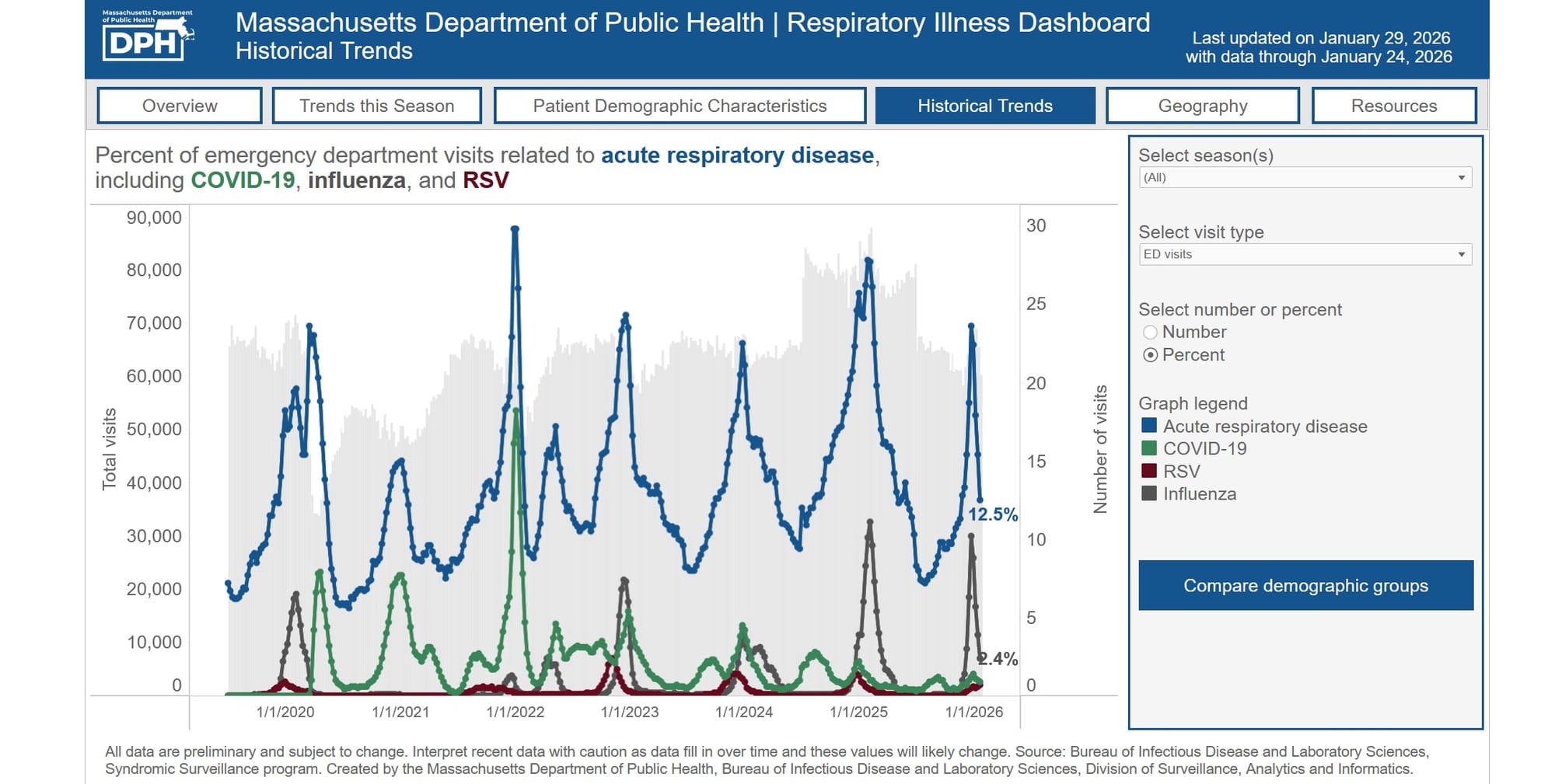
In Massachusetts, there have been three pediatric and 29 adult deaths from flu. However, state health officials are actually seeing low numbers for COVID-19, respiratory syncytial virus (RSV), and other respiratory illnesses, with two possible COVID-associated deaths and one RSV-associated death in individuals younger than 18 years.
According to the Massachusetts Department of Public Health, the number of emergency room visits has dropped from the beginning of 2026 when they were at an all-time high. The latest numbers — from the week of Jan. 18 to Jan. 24 — saw an estimated 12.5% of visits focused on acute respiratory illness: 0.9% for COVID-19; 2.4% for influenza; and 0.7% for RSV.
DPH states that for this time of year, those are “low” numbers in terms of acute respiratory illness and RSV and “very low” for COVID.
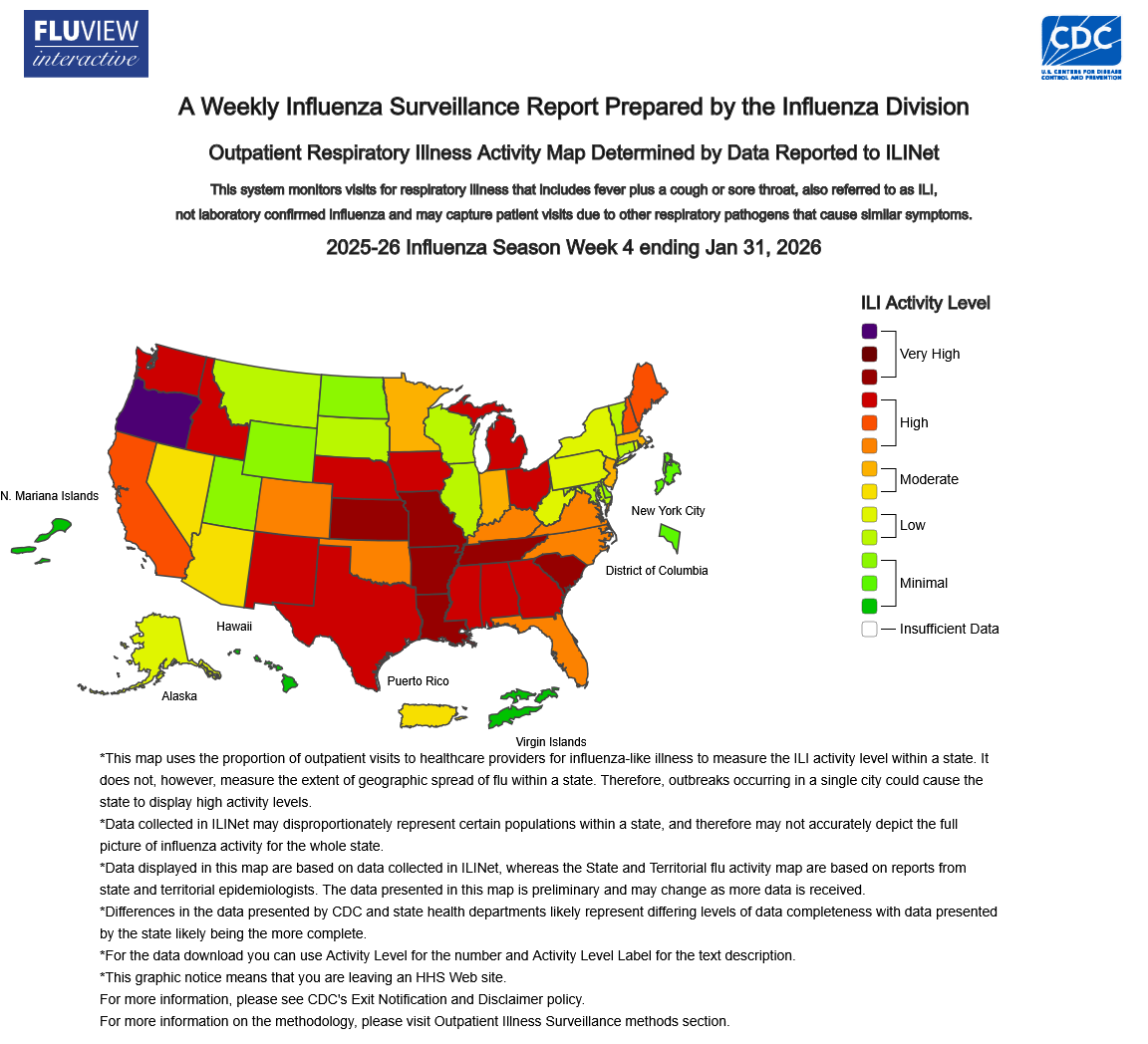
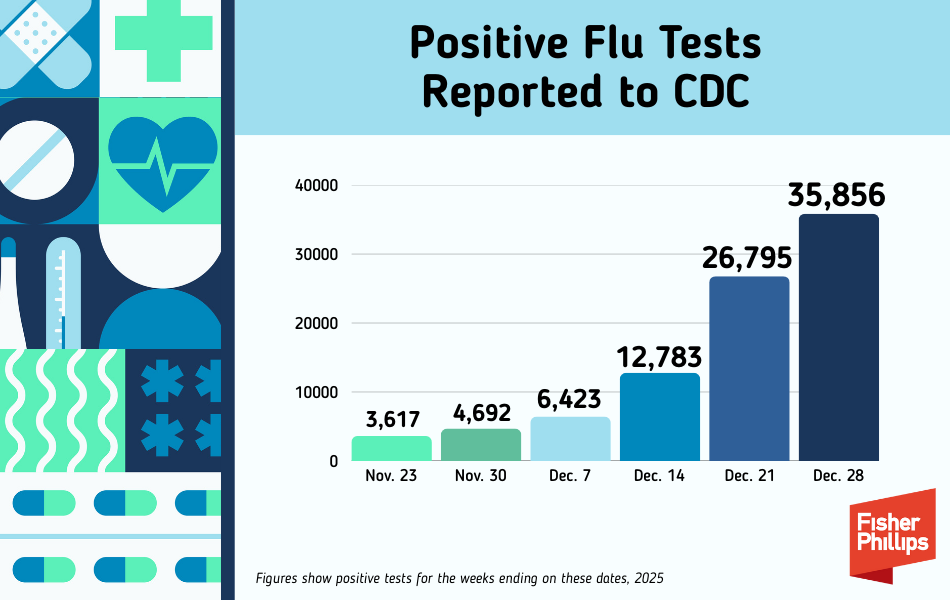
In comparison to past seasons, however, the flu has hit hard. During the week of Dec. 21-Dec. 27 alone, emergency departments saw 65,488 visits, 10.2% of which were diagnosed as flu.
Historically, that’s the second highest year for flu visits. Only the week of Feb. 2-8, 2025, was worse, with 11.1% of visits being related to flu. In the past five years, the DPH recorded its lowest flu season in 2021.
Flu season is typically from October to May, with December through February being the peak.
State officials say it’s not too late to get a flu or COVID vaccine.
“This is a moment for clarity, urgency, and action,” said Public Health Commissioner Dr. Robbie Goldstein in early January. “These viruses are serious, dangerous, and life-threatening. We are seeing children who are seriously ill, families grieving devastating losses, and hospitals under capacity strain. There is a simple, effective, and available way to address these concerns: vaccines. They can prevent serious illness and hospitalization.”
Where we are, according to one health official
We recently asked Dr. Ana Maria Bensaci, an epidemiologist at MelroseWakefield Hospital, some questions about the flu. Here’s what she had to say:
How bad is this flu season compared to others, in your opinion? Better, worse, about the same?
This flu season seems to be driven by a particular variant strain, a type of virus H3N2 subclade K. This may cause people to have less immunity against it.
There’s been a lot of talk about the type A mutation of the flu and how bad that is. Do mutations happen often? Should the public be worried about this one? Is it just part of a natural cycle?
This is a drift, not a shift in the virus. In other words, the virus normally evolves to evade immunity, but it is the same subtype of influenza that we have had for a long time. Antiviral drugs should continue to work against this virus as it has before, and based on information from other countries, the vaccine is working as expected reducing the risk of hospitalization and severe infection.
How effective is the flu vaccine against the “superflu”...the type A mutation? Should people still get the vaccine? Also, what IS the best time to get a flu vaccine? Is there a period of it’s too early or it’s too late?
The vaccine greatly reduces the risk of having a severe episode, reduces the risk of hospitalization and complications from influenza. Even if the vaccine isn’t a perfect match, it substantially lowers the risk of severe illness, hospitalization, and death. Think of it like a seatbelt: it may not prevent every infection, but it greatly reduces the worst outcomes.
We are just at the beginning of the season, now is a good time to take the vaccine for people who have not been vaccinated so far. We want to give the body enough time to get the immunity against it before there is flu circulating, so usually by end of October, but as soon as the vaccine is available is a good time.
COVID really made people tighten up how they took care of themselves (handwashing, wearing masks, etc.). Have people pretty much let that go? Are we still on that high alert? What can we do to keep ourselves safe, even if we have not been as good about taking those safety measures? Is there an “in-between?”
When the COVID pandemic started, there was a lot of uncertainty about the severity, initially there were not vaccines, no treatments. This is reminiscent of the 1918 Spanish flu, there were no vaccines or medications at that time, but the response included isolation, quarantine, good hygiene practices, and the use of masks. These interventions were as valid as they are now.
Prevention fatigue is real, and reduced vaccination plus relaxed hygiene increases spread.
Practical “middle-ground” steps work: Stay home when sick, especially with fever or acute respiratory symptoms. Wear a mask if you must be around others while recovering or caring for someone ill. Wash hands regularly and avoid touching your face. Improve indoor air: open windows, use portable HEPA filters where feasible.
People may not be aware that influenza kills thousands every year, and vaccination is still our best preventative tool, everyone 6 months or above should be vaccinated. This is the best way to protect ourselves and those around us.
Do you think there could be other mutations of flu and how prepared are we to take that on, as a public health system?
Global surveillance runs year-round to track circulating strains, severity, and antiviral resistance. This data informs the annual vaccine formulation and guides clinical recommendations. Sustained funding for surveillance, lab capacity, and vaccination programs is essential to keep pace with viral evolution and to respond quickly to outbreaks.
Are we at the stage where we will probably be seeing more of these types of superflus or other bugs? Is there anything we can do about it or are doing about it?
The risk of emerging or more aggressive infectious diseases is rising due to:
Climate change (altered seasonality and geographic spread of pathogens and vectors); Increased human–animal contact and global travel (more opportunities for zoonotic spillover and rapid spread).
Best defense: evidence-based policy, strong surveillance, rapid response capacity, and high uptake of recommended vaccines and treatments.
Some people have described the superflu as “being hit by a train,” and some say it’s like having COVID. What do you think? I guess I would like to know how folks can distinguish this bug from others. Are there common symptoms to look out for? Should you go to the doc and get tested? Stay at home and nurse yourself? Are there any at-home or over-the-counter remedies you might recommend?
Common flu signs include sudden high fever, strong body aches, headache, extreme tiredness, and cough or sore throat. COVID-19 and RSV can look similar, but influenza tends to cause persistent high fever.
Get tested early. Antiviral medications work best if started within 48 hours of feeling sick, so it is important that patients contact their doctor for advice or seek medical attention if people have conditions that may make them at higher risk for severe illness or if they have severe symptoms.
At home care includes rest, drinking plenty of fluids, and using over-the-counter meds for fever, aches, and cough. Watch for danger signs such as trouble breathing, chest pain, confusion, dehydration, a fever that won’t go down, or symptoms that get better then get worse.
Stay home at least 5 days from when symptoms start and until you’ve been fever-free for 24 hours without fever-reducing medicine. When you go back out, consider wearing a mask for a few more days, especially around older adults, infants, or anyone with health conditions. There is information regarding treatment, please refer to the most recent CDC guideline.